A groundbreaking study published in the British Medical Journal has revealed that Depo Provera users are 5.5 times more likely to develop meningioma brain tumors compared to non-users. This stunning scientific finding has triggered a wave of litigation against Pfizer and related defendants.
Depo Provera (medroxyprogesterone acetate) is a contraceptive injection administered every three months. When used consistently, it's over 99% effective in preventing pregnancy. Key points:

The March 2024 study published in the British Medical Journal represents a watershed moment in understanding the connection between Depo-Provera and brain tumors. This comprehensive research analyzed data from the French National Health Data System, examining 108,366 women, including 18,061 who underwent meningioma surgery. The study's findings were statistically stunning: women using Depo-Provera showed a risk ratio of 5.5, meaning they were more than five times more likely to develop meningiomas compared to non-users. Within the study group, researchers identified nine cases of meningioma among Depo-Provera users out of 18,061 total cases (0.05%), compared to just eleven cases among 90,305 controls (0.01%), demonstrating a clear and significant increase in risk.
The BMJ study carefully differentiated between various hormonal treatments, finding increased risk specifically associated with medrogestone, medroxyprogesterone acetate (Depo-Provera), and promegestone. Notably, the research found no elevated risk with other common hormone treatments such as progesterone, dydrogesterone, and certain hormonal IUDs. This specificity adds credibility to the findings by demonstrating that not all hormone treatments carry the same risks.
Four decades before the 2024 findings, researchers had already identified potential concerns. A pivotal 1983 study published in the European Journal of Cancer & Clinical Oncology discovered high concentrations of progesterone receptors in meningioma cells. This research revealed that meningioma cells contained a greater density of progesterone receptors compared to estrogen receptors, establishing the biological foundation for understanding how hormone-based drugs like Depo-Provera could potentially accelerate tumor growth.
Further validation came through a 1991 study in the Journal of Neurosurgery that explored the effects of mifepristone, an anti-progesterone agent, on meningiomas. The research demonstrated that blocking progesterone could effectively reduce tumor growth, providing additional evidence of progesterone's role in promoting meningioma development. This study essentially confirmed the biological mechanism through which Depo-Provera could influence tumor growth.
The current scientific evidence is particularly compelling due to several key factors. The 5.5 risk ratio found in the 2024 study far exceeds typical associations seen in pharmaceutical research, providing unusually strong statistical support for causation. The biological mechanism is well-understood and documented through multiple studies, showing how synthetic progesterone interacts with tumor cells. Additionally, the temporal relationship between drug exposure and tumor development has been consistently demonstrated across various research efforts.
The extensive scientific evidence spanning four decades raises serious questions about Pfizer's duty to warn. The progression of research from the 1983 identification of progesterone receptors in meningioma cells, through the 1991 confirmation of progesterone's role in tumor growth, to the 2024 epidemiological confirmation of increased risk, suggests that Pfizer had ample opportunity to recognize and warn about potential risks. The company's failure to update warning labels, despite mounting scientific evidence, forms a central argument in current litigation.
These scientific findings have profound implications for patient care and medical decision-making. The clear risk profile established through research, particularly the significant increase in meningioma risk, suggests the need for careful consideration when prescribing Depo-Provera, especially given the availability of alternative contraceptive options with lower risk profiles. The scientific evidence supports arguments that patients should have been informed of these risks to make educated decisions about their contraceptive choices.
The body of scientific evidence provides an unusually strong foundation for litigation. The combination of early mechanistic studies, consistent findings across decades, and the recent high-powered epidemiological study creates a compelling scientific case for the link between Depo-Provera and meningioma development. The clarity and strength of this evidence distinguishes the Depo-Provera litigation from many other pharmaceutical cases where causation may be more tenuous or disputed.

Meningiomas represent the most common type of brain tumor, accounting for approximately 40% of all primary brain tumors. These tumors develop in the meninges, the protective membranes that cover the brain and spinal cord. Their location within these crucial protective tissues makes them particularly concerning, as they can affect various neurological functions depending on their size and specific location within the brain.
Grade I meningiomas, representing approximately 80% of all cases, are considered benign tumors. However, the term "benign" can be misleading, as these tumors can still cause significant health issues. These tumors typically grow slowly, allowing for more treatment options and generally offering a better prognosis. Despite their slower growth rate, Grade I meningiomas can still compress surrounding brain tissue, leading to serious symptoms including headaches, vision problems, and seizures. Treatment often involves careful monitoring, and in many cases, surgical intervention may be necessary if the tumor locations or symptoms warrant it.
Grade II meningiomas present a more complex medical challenge. While still technically non-cancerous, these tumors exhibit more aggressive growth patterns and cellular abnormalities. Treatment becomes more challenging due to their faster growth rate and tendency to recur even after successful initial treatment. Patients with Grade II meningiomas typically require more aggressive treatment approaches, often combining surgery with radiation therapy. The higher recurrence rate means patients need more frequent monitoring and may face multiple surgical interventions throughout their treatment journey.
Grade III meningiomas, though rare at less than 2% of cases, represent the most serious classification. These malignant tumors grow aggressively and can spread to other areas of the brain and body. The rapid growth rate of Grade III meningiomas demands immediate and aggressive intervention, typically involving a combination of surgery, radiation therapy, and sometimes chemotherapy. The prognosis for Grade III meningiomas is generally more guarded, and patients require intensive medical management and close monitoring.
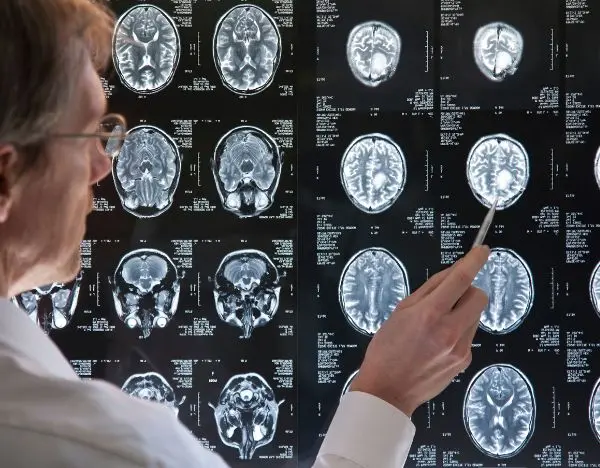
The path to diagnosing a meningioma often begins with symptoms that may seem unrelated to brain tumors. Common initial symptoms include persistent headaches, changes in vision, seizures, and gradual changes in cognitive function. Many patients report experiencing symptoms for months or even years before receiving a definitive diagnosis. Modern imaging techniques, particularly MRI scans, have improved the ability to detect these tumors early, though many are still discovered incidentally during imaging for other conditions.
The primary treatment for symptomatic meningiomas typically involves surgical removal through a procedure called a craniotomy. This highly invasive brain surgery requires removing a portion of the skull to access and remove the tumor. The complexity and risks of surgery vary significantly depending on the tumor's location and size. While some tumors can be completely removed, others in sensitive areas may only be partially resectable, necessitating additional treatments to manage remaining tumor tissue.
Recovery from meningioma treatment, particularly after surgery, requires extensive rehabilitation and monitoring. Patients often face both physical and cognitive challenges during recovery. The rehabilitation period can extend for months or even years, requiring various therapeutic interventions including physical therapy, occupational therapy, and sometimes speech therapy. Long-term monitoring is essential for all grades of meningioma due to the possibility of recurrence.
Living with a meningioma diagnosis significantly affects patients' quality of life, regardless of the tumor's grade. Even with successful treatment, patients often face ongoing challenges including chronic headaches, cognitive changes, and the psychological burden of living with a brain tumor. Many patients require long-term medication management and must make significant lifestyle adjustments to accommodate their condition.
While survival rates for meningioma vary significantly based on tumor grade and location, modern treatment approaches have improved overall outcomes. Grade I tumors generally have excellent survival rates when completely removed, though monitoring is still necessary. Grade II tumors have moderate survival rates but require more vigilant monitoring due to higher recurrence rates. Grade III tumors, despite aggressive treatment, still present significant challenges to long-term survival and require the most intensive medical management.
The comprehensive treatment required for meningiomas often creates substantial financial and emotional burdens for patients and their families. Treatment costs can be extensive, particularly given the need for specialized surgical procedures, ongoing imaging studies, and potential rehabilitation services. The emotional toll of managing a brain tumor diagnosis, combined with uncertainty about potential recurrence, creates significant psychological challenges for patients and their support systems.
The Emerging Landscape of Lawsuits
As of October 2024, the Depo Provera litigation is rapidly evolving across the United States. Multiple Depo Provera Lawsuits have been filed in various jurisdictions, with new cases emerging weekly as more women become aware of the connection between their meningioma diagnoses and Depo Provera use. The litigation gained significant momentum following the March 2024 British Medical Journal study that established a compelling scientific link between the contraceptive and brain tumor development.
Strategic Focus on Philadelphia Courts
Philadelphia has emerged as a pivotal venue for Depo Provera lawsuits, particularly within the Philadelphia Court of Common Pleas. This court's selection is strategic, given its experienced judiciary in handling complex mass tort and product liability cases. The court's Complex Litigation Center (CLC) has earned a reputation for efficiently managing large-scale pharmaceutical cases. Additionally, Philadelphia's connection to the litigation is strengthened by defendant Viatris Inc.'s headquarters in Canonsburg, Pennsylvania, providing a jurisdictional basis for filing cases in the state.
Formation of Federal Multidistrict Litigation
The federal court system is moving toward establishing a Multidistrict Litigation (MDL) to handle the growing number of Depo Provera cases. Currently, there are only three Depo Provera Lawsuits in federal court, but this number is expected to grow significantly. The creation of an MDL would streamline pretrial proceedings, including discovery and preliminary motions, while preserving each plaintiff's right to an individual trial. The relatively small number of current federal cases has temporarily delayed MDL formation, as the Judicial Panel on Multidistrict Litigation typically requires a critical mass of cases before establishing centralized proceedings.
State Court Consolidation Efforts
Parallel to federal proceedings, several states are working to consolidate their Depo Provera cases. Pennsylvania state courts, particularly in Philadelphia, are leading this effort. The state consolidation approach offers certain advantages, including potentially more favorable expert testimony standards and historically sympathetic jury pools. These state-level proceedings may move more quickly than federal cases, potentially establishing important precedents for the broader litigation.
A significant development occurred in October 2024 with the filing of a new Depo Provera Lawsuit in Hamilton County, Indiana. This case highlights the severe health impacts of Depo Provera use, detailing a patient's journey from initial symptoms to multiple surgical interventions. The plaintiff began receiving Depo-Provera injections in 1995 and continued until 2018, experiencing progressively worsening symptoms including dizziness, fatigue, and eventual diagnosis of a large meningioma requiring extensive treatment.
Focus on Failure to Warn Claims
The current litigation strategy centers primarily on failure to warn claims against Pfizer and related defendants. These claims argue that despite mounting scientific evidence dating back to 1983, Pfizer failed to adequately warn patients and healthcare providers about the risk of meningioma associated with Depo Provera use. The addition of meningioma warnings to European product labels, while similar warnings remained absent in the United States, strengthens these claims.
Defendant Response and Legal Strategy
Pfizer and other defendants have begun formulating their defense strategy, particularly focusing on the time gap between early studies and definitive epidemiological evidence. However, the defendants face challenges in explaining why European labels contained meningioma warnings while U.S. labels did not. Pfizer's April 2024 public statement acknowledged awareness of the potential risk and indicated plans to update product labels, though this acknowledgment may strengthen plaintiffs' claims regarding prior failure to warn.
Role of Generic Manufacturers
The litigation has expanded to include claims against manufacturers of generic versions of Depo Provera. A unique aspect of this litigation involves Pfizer's use of subsidiaries Greenstone and Prasco to market "authorized generic" versions of the drug. This corporate structure may allow plaintiffs who used generic versions to pursue Depo Provera Lawsuits against Pfizer, circumventing typical limitations on generic manufacturer liability.
Current Settlement Discussions
While still in early stages, preliminary settlement discussions are being monitored closely. The strength of the scientific evidence, combined with Pfizer's substantial financial resources and the serious nature of the injuries involved, suggests potential for significant settlement values. However, formal settlement negotiations likely won't begin until more cases are filed and consolidated, establishing a clearer picture of the litigation's scope.
Future Litigation Timeline
The litigation is expected to follow a typical mass tort timeline, with initial cases being filed throughout 2024 and early 2025. Once an MDL is established, the court will likely select bellwether cases for early trials, which will help establish settlement values for different categories of Depo Provera Lawsuits. The selection of these bellwether cases and their outcomes will significantly influence the direction of the broader litigation.

Pfizer's Central Role as Primary Defendant
Pfizer Inc. stands as the principal defendant in the Depo Provera litigation, holding primary responsibility as the current New Drug Application (NDA) holder. Since acquiring Pharmacia & Upjohn in 2002, Pfizer has maintained direct control over Depo-Provera's production, labeling, and safety information. The company's position as one of the world's largest pharmaceutical manufacturers, with substantial financial resources particularly bolstered by Covid vaccine profits, makes it the primary target for litigation. Pfizer's deep pockets, estimated at over $150 billion in value, significantly influence the litigation strategy as they have the clear ability to pay substantial settlements without financial strain.
Viatris Inc.'s Complex Corporate Evolution
Viatris Inc. emerged through a significant corporate restructuring in 2020, formed by the merger of Upjohn, Greenstone, and Mylan N.V. The company's role in the Depo Provera litigation stems from its participation in both the distribution and sale of the drug and its "authorized generic" versions. Viatris's headquarters in Canonsburg, Pennsylvania, provides a strategic advantage for plaintiffs, allowing them to file cases in Pennsylvania state courts. This corporate connection to Pennsylvania has made Philadelphia's Court of Common Pleas a preferred venue for many Depo Provera lawsuits.
Greenstone LLC's Role as Pfizer's Subsidiary
Greenstone LLC's position in the litigation is particularly noteworthy as a wholly-owned subsidiary of Pfizer specifically created to serve as an "authorized generic" distributor. The company produced and distributed versions of Depo Provera that were chemically identical to the branded version but marketed without brand labeling. This corporate structure raises significant legal questions about liability and responsibility for warning labels, as Greenstone operated under Pfizer's infrastructure with personnel reporting directly to Pfizer. Their role in distributing "authorized generics" may help plaintiffs overcome typical limitations on generic manufacturer liability.
Prasco Laboratories' Distribution Network
Prasco Labs enters the litigation as another "authorized generic" distributor, having marketed Depo Provera as a generic product while maintaining its chemical composition identical to the branded version. The company's relationship with Pfizer involved marketing these authorized generic versions without altering either the chemical composition or labeling. This arrangement potentially exposes both companies to liability for failing to provide adequate warnings about meningioma risks, regardless of whether patients received the branded or generic version of the medication.
Historical Responsibility of Pharmacia & Upjohn
Pharmacia & Upjohn's role in the litigation stems from its position as the original NDA holder for Depo Provera before Pfizer's acquisition. The company faces allegations of failing to address safety issues with Depo Provera during its period of control. Though now part of Pfizer, Pharmacia & Upjohn's historical actions and decisions regarding safety warnings and risk assessment remain relevant to the current litigation, particularly concerning what was known about meningioma risks during their period of ownership and control.
Corporate Interconnections and Liability
The complex web of corporate relationships among these defendants creates unique legal considerations in the Depo Provera litigation. Pfizer's control over its subsidiaries and partners, combined with its majority ownership of Viatris, suggests a coordinated distribution network that benefited from consistent labeling practices across all versions of the product. This corporate structure may actually strengthen plaintiffs' claims by demonstrating Pfizer's ability to influence warning labels across both branded and generic versions of the medication.
Impact on Generic Drug Users' Claims
The corporate relationships between these defendants, particularly Pfizer's control over authorized generic manufacturers, may provide a legal pathway for users of generic Depo Provera to pursue claims. Typically, users of generic medications face significant hurdles in failure-to-warn cases due to federal preemption rules. However, the authorized generic structure used by Pfizer through Greenstone and Prasco may allow these claims to proceed, as these companies essentially operated as extensions of Pfizer rather than truly independent generic manufacturers.
Financial Considerations and Settlement Capacity
The financial strength of these defendants, particularly Pfizer, significantly influences the litigation's potential outcomes. Pfizer's substantial resources ensure ability to pay meaningful settlements while also potentially funding a robust defense. The other defendants' financial positions and corporate relationships with Pfizer may affect settlement strategies and the ultimate resolution of these cases.
Strategic Implications for Plaintiffs
Understanding the relationships between these defendants proves crucial for plaintiffs' attorneys in developing effective litigation strategies. The corporate structure allows for various approaches to establishing liability, potentially expanding the pool of eligible plaintiffs to include users of both branded and generic versions of Depo Provera. This comprehensive approach to defendant liability may ultimately lead to more favorable outcomes for plaintiffs in both individual cases and potential global settlements.
Minimum Exposure Requirement
Law firms have established a minimum threshold of two Depo Provera injections to qualify for litigation. This requirement stems from careful consideration of the scientific evidence regarding dose-response relationships. While some law firms initially considered requiring four injections, the compelling nature of the latest scientific evidence, particularly the 5.5 risk ratio demonstrated in the 2024 BMJ study, supports the two-injection minimum. This threshold acknowledges that even limited exposure to the drug's synthetic progesterone could potentially trigger tumor development in susceptible individuals.
Medical Documentation of Drug Usage
Establishing proof of Depo Provera use requires comprehensive medical documentation. Acceptable forms of evidence include medical records from prescribing physicians, injection administration records, pharmacy records, and insurance billing documentation. The timing and duration of Depo Provera use must be clearly documented, as this information helps establish the connection between drug exposure and subsequent tumor development. Insurance records have proven particularly valuable in cases where direct medical records may be incomplete or difficult to obtain.
Meningioma Diagnosis Requirements
A confirmed diagnosis of meningioma or other qualifying brain tumor represents a fundamental requirement for eligibility. The diagnosis must be properly documented through medical records, including imaging studies (such as MRI or CT scans), pathology reports if surgery was performed, and detailed medical records from treating physicians. The timing of the diagnosis relative to Depo Provera use is crucial, though there is no strict time limitation given the generally slow-growing nature of these tumors.
Exclusionary Medical Conditions
Several medical conditions can exclude potential claimants from the litigation. These exclusions exist because certain conditions represent alternative explanations for tumor development. Key exclusionary conditions include:
Genetic Conditions
Neurofibromatosis type 2 (NF2) serves as a primary exclusion due to its strong association with meningioma development. Other excluding genetic conditions include Gorlin syndrome, multiple endocrine neoplasia type 1 (MEN1), Turcot syndrome, Lynch syndrome, Li-Fraumeni syndrome, Cowden syndrome, and Von Hippel-Lindau disease. These conditions are excluded because they independently increase the risk of developing meningiomas.
Prior Radiation Exposure
Previous exposure to ionizing radiation, particularly cranial radiation therapy, represents another significant exclusionary factor. Radiation exposure has a well-documented association with meningioma development, making it difficult to establish Depo Provera as the primary cause of tumor growth in these cases.
Age Considerations
While there is no strict age limit for eligibility, the age at which a claimant received Depo Provera injections and subsequent tumor diagnosis may influence case evaluation. Age considerations help establish the plausibility of the causal relationship between drug exposure and tumor development.
Timing of Claims
The statute of limitations for filing claims varies by state but may be extended due to two key legal principles. The discovery rule delays the start of the limitations period until a plaintiff reasonably should have known about both the injury and its connection to Depo Provera. Additionally, the doctrine of fraudulent concealment may toll the statute of limitations based on allegations that Pfizer actively concealed the risks associated with the drug.
Strength of Individual Depo Provera Lawsuits
Beyond basic eligibility criteria, several factors influence the strength of individual Depo Provera Lawsuits. These include the duration of Depo Provera use, the severity and grade of the meningioma, the extent of medical interventions required, and the impact on the claimant's quality of life. Cases involving longer drug exposure periods, higher-grade tumors, or more extensive medical interventions typically present stronger Depo Provera Lawsuits.
Documentation Requirements
Successful Depo Provera Lawsuits require extensive documentation beyond basic proof of drug use and diagnosis. Valuable documentation includes:
Role of Medical Experts
Expert medical testimony plays a crucial role in establishing Depo Provera Lawsuit eligibility. Medical experts help establish the causal connection between Depo Provera use and tumor development, particularly in cases where other risk factors may be present. Their evaluation of medical records and scientific literature helps strengthen individual claims.
Geographic Considerations
While eligibility criteria remain largely consistent nationwide, the choice of venue can significantly impact a claim's viability. Some jurisdictions, particularly Philadelphia's Court of Common Pleas, may offer more favorable conditions for pursuing these Depo Provera Lawsuits. Geographic considerations may influence where claims are filed, regardless of where the claimant resides.
Overview of Settlement Projections
Settlement valuations in the Depo Provera litigation reflect the serious nature of meningioma injuries and Pfizer's substantial financial resources. Early projections suggest a tiered settlement structure, with compensation varying significantly based on tumor grade and severity of complications. While it's still early in the litigation process, analysis of comparable brain tumor cases and Pfizer's history of mass tort settlements provides insight into potential compensation ranges.
Grade I Meningioma Settlement Projections
For Grade I meningioma cases, current projections estimate settlements between $275,000 and $500,000. These benign but still serious tumors typically require surgical intervention and ongoing monitoring. The settlement range accounts for various factors including successful tumor removal, recovery time, and the need for continued medical surveillance. Even though these tumors are classified as benign, their location in the brain and the invasive nature of required treatments justify substantial compensation.
Grade II Meningioma Valuations
Grade II meningioma cases are expected to command higher settlement values due to their more aggressive nature and increased treatment complexity. These cases often involve multiple surgical interventions and higher recurrence rates. The combination of more extensive medical treatment, increased risk of complications, and greater impact on quality of life suggests settlement values potentially ranging from $500,000 to $750,000, depending on specific case factors.
Grade III Malignant Cases
The most serious cases involving Grade III malignant meningiomas could potentially settle for over $1 million. These aggressive tumors require immediate and extensive intervention, often including multiple surgeries, radiation therapy, and ongoing treatment. The life-threatening nature of these tumors, combined with their significant impact on life expectancy and quality of life, justifies the highest settlement values in the litigation.
Impact of Medical Interventions
The extent and complexity of required medical interventions significantly influence settlement values. Cases involving multiple surgical procedures, extensive radiation therapy, or experimental treatments typically command higher settlements. The need for ongoing medical care and future medical expenses also factors into settlement calculations, particularly in cases where tumors have recurred or require continuous monitoring.
Long-term Complications and Prognosis
Settlement values are substantially affected by the presence and severity of long-term complications. Cases involving permanent neurological deficits, cognitive impairment, or the need for lifetime care generally receive higher compensation. The impact on the patient's ability to work, maintain relationships, and engage in daily activities plays a crucial role in valuation calculations.
Age Considerations in Settlement Valuation
The age of the plaintiff at diagnosis significantly influences settlement amounts. Younger plaintiffs typically receive higher settlements due to longer life expectancy with complications, greater lifetime earning potential loss, and more years of required medical monitoring. However, older plaintiffs with dependent care responsibilities or established careers may also receive substantial settlements based on their specific circumstances.
Economic Damages Components
Settlement calculations include various forms of economic damages. These encompass past and future medical expenses, lost wages, lost earning capacity, and the cost of ongoing care needs. The documentation of these expenses and projected future costs plays a crucial role in determining settlement values. Cases with well-documented economic losses typically receive higher settlements.
Non-Economic Damages Considerations
Pain and suffering, emotional distress, and loss of quality of life represent significant components of settlement values. The psychological impact of living with a brain tumor, including anxiety about recurrence and the emotional toll of treatment, factors heavily into non-economic damage calculations. Cases with clear evidence of significant lifestyle changes or emotional trauma may receive higher compensation for these intangible losses.
Pfizer's Financial Capacity
Pfizer's substantial financial resources, particularly following Covid-19 vaccine profits, suggest the company has ample ability to pay significant settlements. This financial capacity, estimated at over $150 billion in value, indicates that settlement amounts won't be constrained by defendant resources, unlike many other mass tort cases. This factor could lead to more generous settlement offers across all injury categories.
Geographic Variations
Settlement values may vary by jurisdiction. Cases filed in historically plaintiff-friendly venues like Philadelphia may command higher settlements. Additionally, state-specific laws regarding damages caps and the admissibility of certain types of evidence can influence local settlement values.
Trial outcomes and evolving scientific evidence may influence later settlements
Early settlements may differ from later ones as the litigation evolves. Initial settlements often set benchmarks for future cases, while trial outcomes and evolving scientific evidence may influence later settlements. The timing of settlement in relation to potential trial dates can also affect settlement amounts.
Impact of Scientific Evidence
The strength of scientific evidence linking Depo Provera to meningiomas, particularly the 5.5 risk ratio identified in the 2024 BMJ study, supports higher settlement values. This compelling scientific evidence strengthens causation arguments and may lead to more favorable settlement terms across all case categories.
If you've taken Depo Provera and have been diagnosed with a meningioma or other brain tumor, time is critical for protecting your legal rights. Our experienced pharmaceutical litigation team offers free consultations to evaluate your case. Don't let the statute of limitations expire on your Depo Provera Lawsuit - reach out now to understand your options for compensation.
Can I file a Depo Provera Lawsuit if I took generic Depo Provera? Yes, you may still qualify for a Depo Provera Lawsuit even if you used generic Depo Provera. This is because Pfizer used its subsidiaries, Greenstone and Prasco, to market "authorized generic" versions of the drug that were chemically identical to the brand-name product. This corporate structure allows Depo Provera Lawsuits against Pfizer regardless of whether you used brand-name or generic versions.
How long do I have to file a Depo Provera lawsuit? The discovery rule in most states means the statute of limitations begins when you discovered or reasonably should have discovered the connection between Depo Provera and your meningioma. Given the recent publication of the 2024 BMJ study, most potential Depo Provera Lawsuits are still within the statute of limitations if filed promptly.
Will I need to testify in court? Most plaintiffs in pharmaceutical mass tort litigation never need to appear in court. The majority of work involves submitting medical records and documentation, which is primarily handled by your attorneys. If the litigation results in a global settlement, most cases will resolve without trial testimony.
Does it matter how long ago I took Depo Provera? There is no strict time limit on when you took Depo Provera. The key factors are establishing that you received at least two injections and subsequently developed a meningioma. Given the slow-growing nature of these tumors, cases involving Depo Provera use from many years ago may still qualify.
What if I'm still taking Depo Provera? If you're currently taking Depo Provera, consult with your healthcare provider about alternative birth control options. The decision to continue or discontinue the medication should be made with your doctor's guidance, but you may still pursue a Depo Provera Lawsuit if you've been diagnosed with a meningioma.
What documentation will I need to file a Depo Provera Lawsuit? While attorneys can help gather records, it's helpful to collect medical records showing Depo Provera prescriptions, insurance records documenting the injections, and all medical documentation related to your meningioma diagnosis and treatment.
How long does the legal process take? Mass tort pharmaceutical litigation typically takes several years to resolve. However, once consolidated into an MDL or state court proceedings, cases often move toward settlement negotiations after initial bellwether trials establish case values.
What if my loved one died from a meningioma after taking Depo Provera? The estate of a deceased person may file a wrongful death claim if there's evidence linking Depo Provera use to the development of a fatal meningioma. These cases often have higher potential settlement values due to the severity of the outcome.
Do I need money upfront to file a Depo Provera Lawsuit? Most law firms handling Depo Provera cases work on a contingency fee basis, meaning they only get paid if they win your case. Initial consultations are typically free, and you don't need to pay any upfront legal fees.
What if I'm not sure when I received Depo Provera injections? Your attorneys can help obtain medical and pharmacy records to document your Depo Provera use. Insurance records, medical charts, and pharmacy databases can often provide this information even if you don't remember exact dates.
Can I file a Depo Provera Lawsuit if my tumor was successfully removed? Yes, you can still pursue compensation even if your tumor was successfully removed. The invasive nature of brain surgery, recovery time, and ongoing monitoring requirements all factor into potential compensation, regardless of the surgery's outcome.
What sets the Depo Provera litigation apart from other drug lawsuits? The unusually strong scientific evidence (5.5 risk ratio), combined with Pfizer's significant financial resources and the serious nature of brain tumors, makes this litigation particularly compelling compared to many other pharmaceutical cases.





